Neuroscience of ADHD
Neuroscience Of ADHD: Key Brain Regions
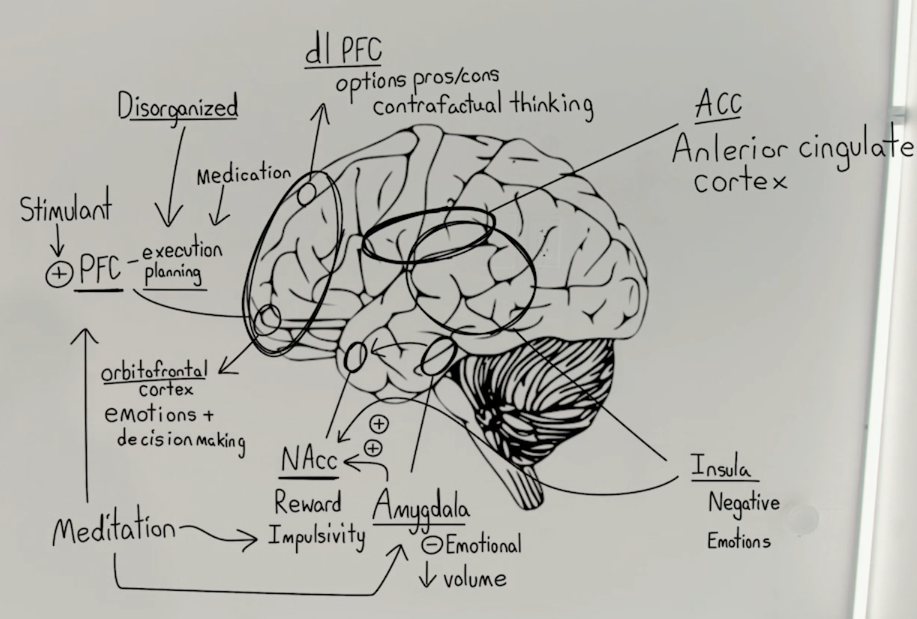
ADHD involves several key brain regions, each contributing to different aspects of the disorder:
-
Amygdala and Insula:
- Smaller in volume in ADHD brains
- Associated with increased emotional responsiveness
-
Nucleus Accumbens:
- Part of the dopamine reward circuitry
- More strongly influenced by emotions in ADHD
-
Prefrontal Cortex (PFC):
- Involved in execution and planning of behavior
- Includes Orbital Frontal Cortex (emotion regulation and decision-making)
- Includes Dorsolateral PFC (weighing options, pros/cons)
-
Anterior Cingulate Cortex (ACC):
- Connects PFC with emotional circuitry
- Weaker in ADHD brains
“So the cool thing about the neuroscience of ADHD is that a lot of the deficits that we see actually map onto the brain. And once we understand what’s going on in the brain, it gives us a roadmap for how to fix things.”
- How might understanding the neuroscience of ADHD lead to more targeted treatments?
- What are the implications of the brain differences in ADHD for cognitive and emotional functioning?
- How can this neurological understanding help in developing personalized interventions for individuals with ADHD?
Brain Plasticity in ADHD, Neuroimaging in ADHD, Neurodevelopmental Aspects of ADHD
Emotional Regulation in ADHD
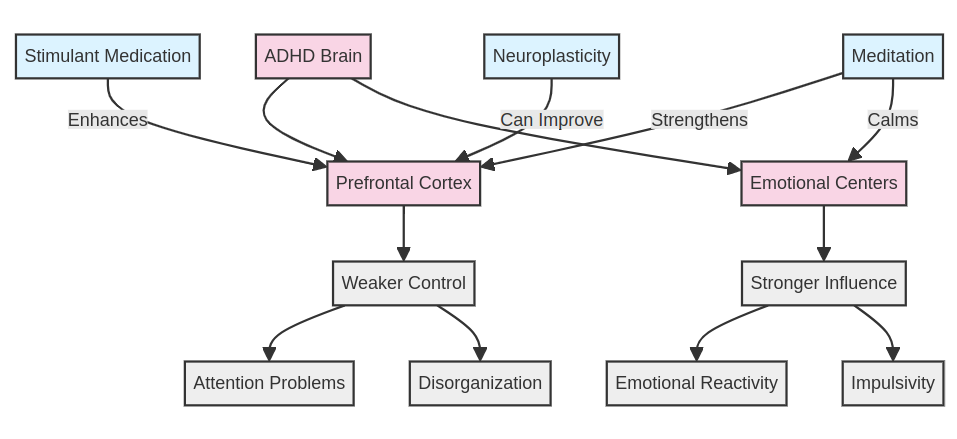
People with ADHD often struggle with emotional regulation due to specific brain differences:
- Smaller amygdala and insula volumes correlate with increased emotional responsiveness
- Stronger connections between emotional centers (amygdala/insula) and reward center (nucleus accumbens)
- Weaker connections between prefrontal cortex and emotional circuitry via the anterior cingulate cortex
These differences can lead to more impulsive emotional reactions and difficulties in emotional control.
“So something that we’ll see in people with ADHD is that sometimes their emotions get the better of them, they kind of become a little bit impulsive.”
- What strategies can be developed to help individuals with ADHD improve their emotional regulation?
- How might understanding the neurological basis of emotional dysregulation in ADHD impact treatment approaches?
- What role might mindfulness or cognitive-behavioral techniques play in addressing these emotional challenges?
Emotional Intelligence in ADHD, Impulse Control Strategies, Cognitive-Behavioral Therapy for ADHD
Executive Function and ADHD
Executive function deficits in ADHD are linked to the prefrontal cortex and its connections:
- Difficulties in planning, organization, and task execution
- Challenges in weighing options and decision-making
- Weaker “brakes” on impulsive thoughts and behaviors
The prefrontal cortex acts as the brain’s “brakes,” which are less effective in ADHD.
“So if we think about planning tasks and executing on them, that’s what our frontal lobes do. So our prefrontal cortex is important for that.”
- How can individuals with ADHD develop strategies to compensate for executive function deficits?
- What role might external supports or technology play in enhancing executive function for those with ADHD?
- How might understanding these deficits change the way we approach education and workplace accommodations for individuals with ADHD?
Executive Function Training, Compensatory Strategies for ADHD, Technology Aids for ADHD
Stimulant Medication Mechanism in ADHD
Stimulant medications work counterintuitively in ADHD by enhancing prefrontal cortex function:
- Stimulants increase the “braking” power of the prefrontal cortex
- This enhanced control helps regulate attention and impulses
- The medication doesn’t slow down thinking, but rather improves control over thoughts and behaviors
“Well, it turns out that what’s what stimulant medications do is actually stimulate the frontal cortex. So what we’re actually boosting the signal of is our ability to control the rest of our brain.”
- How does understanding the mechanism of stimulant medications help in addressing concerns about their use?
- What are the implications of this understanding for developing new ADHD treatments?
- How might this knowledge inform non-pharmacological approaches to enhancing prefrontal cortex function in ADHD?
Neuropharmacology of ADHD, Non-Stimulant ADHD Treatments, Cognitive Enhancement in ADHD
Neuroplasticity and ADHD
The brain’s ability to change over time impacts ADHD symptoms and treatment:
- Some individuals (10-25%) may “grow out” of ADHD as their frontal lobes develop
- Meditation and other interventions may strengthen specific brain areas and connections
- Different types of meditation may target specific ADHD-related brain deficits
“About 10 to 25% of people will actually grow out of ADHD to some degree. And how is that possible? What happens is we age what happens as we age is that the frontal lobes actually strengthen”
- How can understanding neuroplasticity in ADHD inform long-term treatment strategies?
- What role might targeted cognitive training play in enhancing neuroplasticity for individuals with ADHD?
- How might early interventions leverage neuroplasticity to improve long-term outcomes for individuals with ADHD?
Brain Training for ADHD, Meditation and ADHD, Developmental Trajectories in ADHD
Tailored Interventions for ADHD
Understanding the neuroscience of ADHD allows for more personalized and targeted interventions:
- Different meditation techniques can address specific ADHD-related brain deficits
- Interventions can be tailored based on an individual’s particular ADHD symptom profile
- Treatment plans can target specific brain regions or connections that are most affected
“So we can even see how tailoring our meditative technique can target particular shortcomings in the brains of people with ADHD.”
- How can clinicians use neurological insights to create more effective, personalized treatment plans for ADHD?
- What role might emerging technologies play in assessing individual neurological profiles and tailoring interventions?
- How might this approach to tailored interventions change the way we think about ADHD as a spectrum of related but distinct neurological differences?
Personalized Medicine in ADHD, Neurofeedback for ADHD, ADHD Subtype-Specific Interventions